Pain Control After Surgery
A Patient's Guide
|
Purpose of this information:
This information talks about pain relief after surgery. It explains the
goals of pain control and the types of treatment you may receive. It also
shows you hot to work with your doctors and nurses to get the best pain
control
Reading this information should help you:
- Learn why pain control is important for your recovery as well as your
comfort.
- Play an active role in choosing among options for treating your pain.
|
What is pain?
Pain is an uncomfortable feeling that tells you something may be wrong in
your body. Pain is your body's way of sending a warning to your brain. Your
spinal cord and nerves provide the pathway for messages to travel to and
from your brain and the other parts of your body.
Receptor nerve cells in and beneath your skin sense heat, cold, light,
touch, pressure and pain. You have thousands of these receptor cells, most
sense pain and the fewest sense cold. When there is an injury to your body -
in this case surgery - these tinny cells send messages along nerves into
your spinal cord and then up to your brain. Pain medicine blocks these
messages or reduces their effect on your brain.
Sometimes pain may be just a nuisance, like a mild headache. At other
times, such as after an operation, pain that doesn't go away - even after
you take pain medicine - may be a signal that there is a problem. After your
operation, your nurses and doctors will ask you about your pain because they
want you to be comfortable, but also because they want to know if something
is wrong. Be sure to tell your doctors and nurses when you have pain. |
Treatment Goals
People used to think that severe pain after surgery was something they
"just had to put up with." But with current treatments, that's no longer
true. Today, you can work with your nurses and doctors before and after
surgery to prevent or relieve pain. |
Pain Control Can Help You:
- Enjoy greater comfort while you heal.
- Get well faster. With less pain, you can start walking, do your
breathing exercises, and get your strength back more quickly. You may even
leave the hospital sooner.
- Improve your results. People whose pain is well-controlled seem to do
better after surgery. They may avoid some problems (such as pneumonia and
blood clots) that affect others.
|
Pain Control: What are the options?
Both drug and non-drug treatments can be successful in helping to prevent
and control pain. The most common methods of pain control are described
within this booklet. You with your doctors and nurses will decide which ones
are right for you. Many people combine two or more methods to get greater
relief.
Don't worry about getting 'hooked' on pain medicines. Studies show that
this is very rare - unless you already have a problem with drug abuse. |
Pain Control Methods You May Be Using
To get the best results, work with your doctors and nurses to choose the
methods that will work best for you.
Your nurses and doctors want to make your surgery as pain free as they
can. But you are the key to getting the best pain relief because pain is
personal. You are the expert for your pain severity and relief. The amount
or type of pain you feel may not be the same as others feel - even those who
have had the same operation. |
Before Surgery
Drug treatment: Take pain medicine.
Non-drug treatment: Understand what operation the doctor is doing,
why it is being done, and how it will be done. Learn how to do deep
breathing and relaxation exercises. |
During Surgery
Drug treatment: Receive general anesthesia, spinal anesthesia, or
nerve blocks, or take a pain medicine through a small tube in your back
(called an epidural). |
After Surgery
Drug treatment: Take a pain medicine as a pill, shot, or
suppository, or through a tube in your vein or back.
Non-drug treatment: Use massage, hot or cold packs, relaxation,
music or other pastimes to distract you, positive thinking, or nerve
stimulation (TENS). |
What can you do to help keep your pain under control? These seven steps
can help you help yourself.
|
Before Surgery
- Ask the doctor or nurse what to expect.
- Will there be much pain after surgery?
- Where will it occur?
- How long is it likely to last?
Being prepared helps put you in control. You may want to write down
your questions before you meet with your doctor or nurse.
- Discuss the pain control options with your doctors and nurses.
Be sure to:
- Talk with your nurses and doctors about pain control methods that
have worked well or not so well for you before.
- Talk with your nurses and doctors about any concerns you may have
about pain medicine.
- Tell your doctors and nurses about any allergies to medicines you
may have.
- Ask about side effects that may occur with treatment and how to
control them.
- Talk with your doctors and nurses about the medicines you take for
other health problems including over-the-counter medications and vitamin
and mineral supplements. The doctors and nurses need to know, because
mixing some drugs and some pain medicines can cause problems.
- Talk about the schedule for pain medicines in the hospital.
Some people get pain medicines in the hospital only when they call the
nurse to ask for them. Sometimes there are delays and the pain gets worse
while they wait.
Today, two other ways to schedule pain medicines seem to give better
results.
- Giving the pain pills or shots at set times. Instead of waiting
until pain breaks through, you receive medicine at set times during the
day to keep the pain under control.
- Patient controlled analgesia (PCA) may be available in your
hospital. With PCA, you control when you get pain medicine. When you
begin to feel pain, you press a button to inject the medicine through
the intravenous (IV) tube in your vein.
For both ways, your nurses and doctors will ask you how the pain
medicine is working and change the medicine, its dose, or its timing if
you are still having pain.
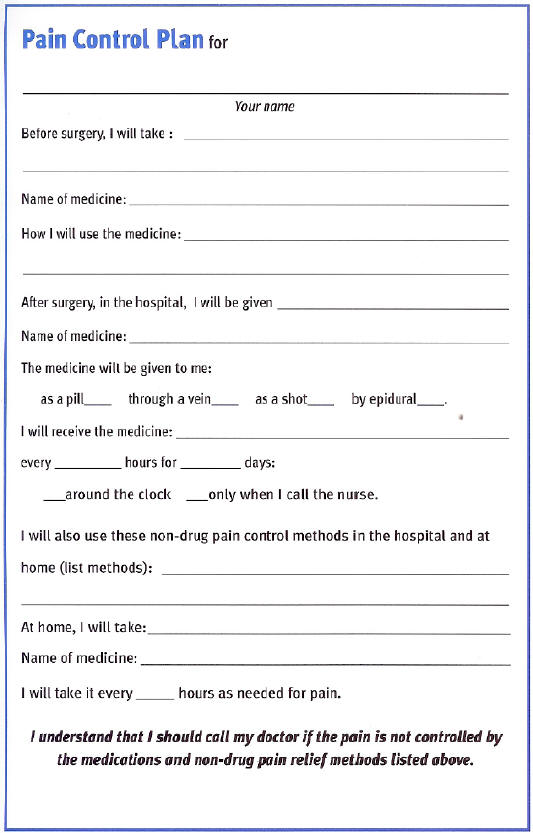
- Work with your doctors and nurses to make a pain control pain.
You can use the form at the end of this page to begin planning for pain
control with your nurses and doctors. They need your help to design the
best plan for you. When your pain control plan is complete, use the form
to write down what will happen. Refer to it after your operation. Then
keep it as a record if you need surgery in the future.
|
After Surgery
- Take (or ask for) pain relief drugs when pain first begins.
- Take action as soon as the pain starts.
- If you know your pain will worsen when you start walking or doing
breathing exercises, or going for rehab therapy, take pain medicine
first. It's harder to ease pain once it has taken hold.
This is a key step in proper pain control.
- Help the doctors and nurses 'measure' your pain.
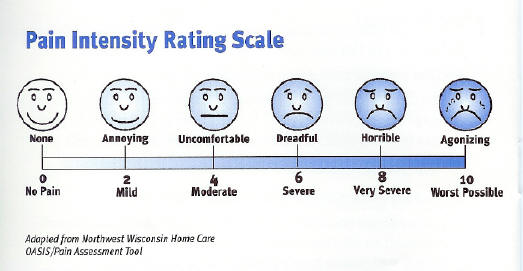
- They will ask you to rate your pain on a scale of 0 to 10. Zero will
represent no pain present and 10 will be the worst pain imaginable. Or
you may choose from a panel of happy to sad faces.
- You may also set a pain control goal (such as having no pain that's
worse than 2 on the scale.
- Reporting your pain as a number helps the doctors and nurses know
how well your treatment is working and whether to make any changes.
- They may ask you to use a 'pain scale' like the one show below.
- They will ask you to describe the pain with words like
sharp, dull, burning, constant,
intermittent, throbbing, aching, and ask if it radiates
to other locations.
- Tell the doctor or nurse about any pain that won't go away.
- Don't worry about being a 'bother'.
- Pain can be a sign of problems with your operation.
- The nurses and doctors want and need to know about it.
Stick with your pain control plan if it is working. Your doctors and
nurses can change the plan if your pain is not under control. You need to
tell the nurses and doctors about your pain and how the pain control plan
is working.
|
 |
Benefits and Risks of Pain Treatment Methods
This information is provided to help you discuss your options with your
doctors and nurses. Sometimes it is best to combine two or more of these
treatments or change the treatments slightly to meet your individual needs.
Your doctors and nurses will discuss this with you. |
Pain Relief Medicines
Nonsteroidal anti-inflammatory drugs: (NASIDs)
Acetaminophen (for example, Tylenol), aspirin, ibuprofen (for example,
Motrin), and other NSAIDs reduce swelling and soreness and relieve mild to
moderate pain.
Benefits:
There is not risk of addiction to these medicines. Depending on how
much pain you have, these medicines can lessen or eliminate the need for
stronger medicines (for example, morphine or another opioid).
Risks:
Most NSAIDs interfere with blood clotting. They may cause nausea,
stomach bleeding, or kidney problems. For severe pain, an opioid usually
must be added.
Opioids:
Morphine, codeine, and other opioids are most often used for acute
pain, such as short-term pain after surgery.
Benefits:
These medicines are effective for severe pain, and they do not cause
bleeding in the stomach or elsewhere. It is rare for a patient to become
addicted as a result of taking opioids for postoperative pain.
Risks:
Opioids may cause drowsiness, nausea, constipation, itching, or
interfere with breathing or urination.
Local anesthetics:
These drugs (for example, bupivacaine) are given, either near the
incision or through a small tube in your back, to block the nerves that
transmit pain signals.
Benefits:
Local anesthetics are effective for severe pain. Injections at the
incision site block pain from that site. There is little or no risk of
drowsiness, constipation, or breathing problems. Local anesthetics reduce
the need for opioid use.
Risks:
Repeated injections are needed to maintain pain relief. An overdose of
local anesthetic can have serious consequences. Average doses may cause
some patients to have weakness in their legs or dizziness.
|
Methods Used to Give Pain Relief
Tablet or liquid
Medicines given by mouth (for example, aspirin, ibuprofen, or opioid
medications such as codeine).
Benefits:
Tablets and liquids cause less discomfort than injections into muscle
or skin and they can work just as well, They are inexpensive, simple to
give, and easy to use at home.
Risks:
These medicines cannot be used if nothing can be taken by mouth or if
you are nauseated or vomiting; sometimes these medicines can be give
rectally (suppository form). There may be a delay in pain relief, since
you must ask for the medicine and wait for it to be brought to you; also,
these medicines take time to wear off.
Injections into skin or muscle
Benefits:
Medicine given by injection into skin or muscle is effective even if
you are nauseated or vomiting.
Risks:
The injection site is usually painful for a short time. Medicines
given by injection are more expensive than tablets or liquids and take
time to wear off. Pain relief may be delayed while you ask the nurse for
medicine and wait for the shot to be drawn up and given.
Injections into vein:
Pain relief medicines are injected into a vein through a small tube,
called an intravenous (IV) catheter. The tip of the tube stays in the
vein.
Benefits:
Medicines given by injection into a vein are fully absorbed and act
quickly. This method is well suited for relief of brief episodes of acute
pain. When a patient controlled analgesia (PCA) pump is used, you can
control your own small, frequent doses of pain medicine.
Risks:
A small tube must be inserted in a vein. If PCA is used, there are
extra costs for pumps and supplies. You must want to use the pump and
learn how and when to give yourself doses of medicine.
Injections into spine:
Medicine is given through a small tube in your back (called an epidural
or intrathecal catheter).
Benefits:
This method works well when you have chest surgery or an operation on
the lower parts of your body.
Risks:
Staff must be specially trained to place a small tube in the back and
to watch for problems that can appear hours after pain medicine is given.
Extra supplies are needed.
|
Non-Drug Pain Relief Methods
These methods can be effective for mild to moderate pain and to boost the
pain-relief effects of drugs. There are no side effects. These techniques
are best learned before surgery.
Patient teaching:
Learning about the operation and the pain expected afterwards (for
example, techniques when coughing or getting out of bed or a chair).
Benefits:
These techniques can reduce anxiety; they are simple to learn, and no
equipment is needed.
Risks:
There are no risks; however, patient attention and cooperation with
staff are required.
Relaxation:
Simple techniques , such as abdominal breathing and jaw relaxation, can
help to increase your comfort after surgery.
Benefits:
Relaxation techniques are easy to learn, and they can help to reduce
anxiety. After instruction, you can use relaxation at any time. No
equipment is needed.
Risks:
There are no risks, but you will need instruction from your nurse or
doctor.
Physical agents:
Hot and cold packs, massage, acupressure, music therapy, and TENS
therapy are some of the non-drug pain relief methods that might be used
following surgery.
Benefits:
In general, physical agents are safe and have no side effects. TENS,
which stands for transcutaneous electrical nerve stimulation, is often
helpful; it is quick to act and can be controlled by the patient.
Risks:
There are no risks related to the use of physical techniques for
managing pain. If TENS is used, there is some cost and staff time involved
for purchasing the machine and instructing patients in its use. Also,
there is only limited evidence to support the effectiveness of TENS for
pain relief in certain situations.
|
Example of Non-drug Pain Relief-Slow Rhythmic Breathing Relaxation
- Breathe in slowly and deeply.
- As you breathe out slowly, feel yourself beginning to relax; feel the
tension leaving your body.
- Now breathe in and out slowly and regularly, at whatever rate is
comfortable for you. You may try abdominal breathing. If you do not know
how to do abdominal breathing, ask your nurse for help.
- To help you focus on your breathing and breathe slowly and
rhythmically:
- Breathe in as you say silently to yourself, "in, two, three."
Breathe out as you say silently to yourself, "out, two, three."
or
- Each time you breathe out, say silently to yourself a word calming
word such as peace or relax.
- You may imagine that you are doing this in a place that is very
calming and relaxing for you, such as lying in the sun at the beach.
- Do steps 1 through 4 only once or repeat steps 3 and 4 for up to 20
minutes.
- End with a slow deep breath. As you breathe out say to yourself "I
feel alert and relaxed."
Additional points: If you intend to do this for more than a few
seconds, try to get a comfortable position in a quiet place. You may close
your eyes or focus on an object. This breathing exercise may be used for
only a few seconds or for up to 20 minutes. |
 |
| |
Resources: Acute Pain Management
Guideline Panel. Pain Control After Surgery, A Patient's Guide. AHCPR Pub.
No. 92-0021. Rockville, :Agency for Healthy Care Policy and Research, Public
Health Service, U.S. Department of Health and Human Services. Feb. 1992.
River Oaks Health System; River Oaks Hospital and Woman's Hospital
Clinical Practice Guideline for Acute Pain Management: Operative or Medical
Procedures for Trauma. The guideline was developed by a private sector,
expert panel made up of doctors, nurses, other health care providers, an
ethicist, and a consumer representative. It was sponsored by the Agency
for Health Care Policy and Research (AHCPR), an agency of the U.S.
Public Health Service.
Pub. No. AHCPR 92-0068 |
| |

Click the links below
to explore the
TOTALLYHIP web site
|

